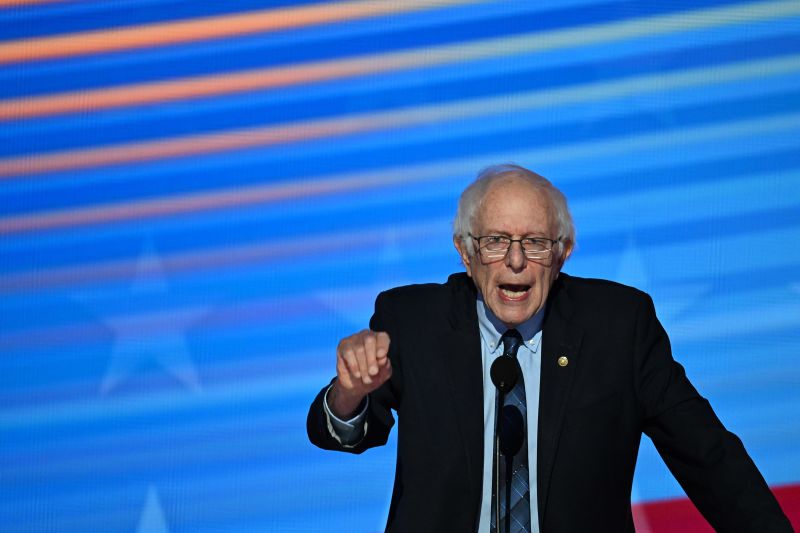
While grilling Novo Nordisk’s chief executive over the price of its blockbuster diabetes and weight-loss drugs, Ozempic and Wegovy, on Tuesday, Sen. Bernie Sanders alleged that 40,000 people a year in the US could die if the company doesn’t make the medicines more affordable.
“From a moral perspective, does it bother you knowing that keeping the price of Ozempic and Wegovy so high in the United States could lead to the preventable deaths of tens of thousands of Americans?” Sanders, chairman of the US Senate Health, Education, Labor and Pensions Committee, asked the Danish drugmaker’s CEO, Lars Fruergaard Jorgensen, citing research from a Yale epidemiologist.
“We are very committed to making sure that Americans have access at an affordable price point for our medicines,” Jorgensen replied. “There’s no thing we would rather see happen.”
It was the latest in a series of hearings Sanders has led with pharmaceutical company CEOs about the price of medicines in the US, which are higher – often by multiple times – than in other wealthy countries. But perhaps no drugs have garnered more attention than Novo Nordisk’s Ozempic, approved for diabetes, and its sister drug, Wegovy, for weight loss and reduction of heart risk. The medicines, also referred to as GLP-1s for the hormone they mimic, are now used by millions of Americans but are still unaffordable and out of reach for many.
Sanders, who launched an investigation of Novo Nordisk in April over what he called “outrageously high prices” for the medications in the US, has focused on the drugs’ comparative cost in other countries: He noted that the list price for a four-week supply of Ozempic is $969 in America, but the drug can be purchased for $155 in Canada, $122 in Denmark and $59 in Germany. Similarly, Wegovy’s list price is $1,349 in the US, but it costs $186 in Denmark, $140 in Germany and $92 in the United Kingdom, he said.
Tuesday’s hearing boiled down to a familiar argument over who is responsible for the US’s higher prices: drug companies that set starting – or “list” – prices or pharmacy benefit managers, the middlemen that negotiate discounts on those list prices in exchange for favorable insurance coverage and access.
Jorgensen said Novo Nordisk pays back about 75% of its medicine sales in rebates, discounts and fees, so the net price it receives is far lower than the list price.
And he argued that when Novo Nordisk has lowered list prices in the past, it’s been penalized by PBMs that profit from discounts, or rebates, on higher prices, in the form of reduced access for patients to its medicines.
“The broad totality is that less patients have access to our medicines when we lowered the price,” Jorgensen told Sen. Maggie Hassan, D-New Hampshire, after she pressed him to reduce list prices.
The Pharmaceutical Care Management Association, the PBMs’ industry group, said in a statement that Jorgensen is trying to shift attention from drugmakers’ moves that keep costs high.
“PBMs are the only entities in the health care system working to mitigate the impact on patients, employers, and taxpayers of Big Pharma’s outrageous prices on blockbuster GLP-1s facing minimal competition,” the association said in a statement. “The critical value of PBMs is being demonstrated in real-time as they are effectively helping plan sponsors navigate a challenging balance between access and cost on GLP-1s for weight loss.”
A pledge from the middlemen
During the hearing, Sanders announced that the committee had obtained written pledges from the largest PBMs to maintain access to Ozempic and Wegovy if Novo Nordisk lowered list prices. The committee simultaneously issued a report about Novo Nordisk’s pricing titled in part: “Greed, greed, greed.”
“That’s new information for me,” Jorgensen told Sanders of the PBMs’ pledges during the hearing. “Anything that will help patients get access to affordable medicine we’ll be happy to look into.”
Jorgensen emphasized, though, that when his company lowered the price of some insulins in the past, “we had our products dropped from formulary coverage, so less patients got access to those insulins. So I have a bit of concern over how this could play out.”
PBMs themselves have been under fire for their role in drug pricing, specifically over the cost of insulin; last week, the Federal Trade Commission sued the three largest – CVS Health’s Caremark, Cigna’s Express Scripts and UnitedHealth Group’s Optum Rx – alleging that they excluded available insulin products with lower prices from coverage in favor of higher-priced insulins that provided higher rebates.
“We let PBMs get away scot-free,” Sen. Tim Kaine, D-Virginia, said later in Tuesday’s hearing, arguing that pharmaceutical companies at least contribute research and “life-saving treatments.”
Sen. Roger Marshall, a Republican from Kansas who is a doctor, called Ozempic a “miracle drug,” saying “Novo Nordisk is not the villain in this story; they’re a hero.”
Concerns over insulin
But while access to insulin is bringing heat to PBMs, it was also the subject of a line of questioning to Jorgensen on Tuesday; Novo Nordisk is one of the three largest manufacturers of the life-saving drug in the world, along with Eli Lilly, which also makes Ozempic and Wegovy’s biggest competitor drugs, Mounjaro and Zepbound.
Multiple senators questioned Jorgensen over Novo Nordisk’s recent announcement that it would stop manufacturing a specific insulin, Levemir, which patients have argued is a critical product they continue to need.
“Any decision to take a product off the market is a very, very difficult decision, and I have to explain why we had to do that,” Jorgensen said. “We, last year, reduced the price for Levemir; we dropped the price, yet to find that PBMs dropped access to Levemir, so much less patients have access to it. … The reality is that the market is disappearing for Levemir because of how it’s contracted.”
- Sign up here to get The Results Are In with Dr. Sanjay Gupta every Friday from the CNN Health team.
Jorgensen said Novo Nordisk has “followed up with” other potential manufacturers of the medicine, “but we have not found anyone interested in manufacturing it.”
Asked by Sen. Tammy Baldwin, a Democrat from Wisconsin, whether Novo Nordisk is shifting manufacturing capacity to the more profitable Ozempic and Wegovy from older insulin products, Jorgensen responded, “we are as committed to insulin as we have always been.”
Ozempic itself may soon face greater pricing pressure; Jorgensen noted in written testimony that the drug will probably be eligible for the next round of Medicare’s drug price negotiations, although rival products from Eli Lilly will not be for another decade. The Centers for Medicare and Medicaid Services is scheduled to announce the names of the next 15 drugs by February. The initial round of negotiations resulted in a 22% reduction in total net spending on 10 drugs.